Imagine waking up every morning gasping for breath - not because of panic, but because a disease is slowly tightening your breathing space. For more than 16 million people with chronic obstructive pulmonary disease (COPD), this is a daily reality. Therefore, it is important to know the information related to COPD!
What is COPD?
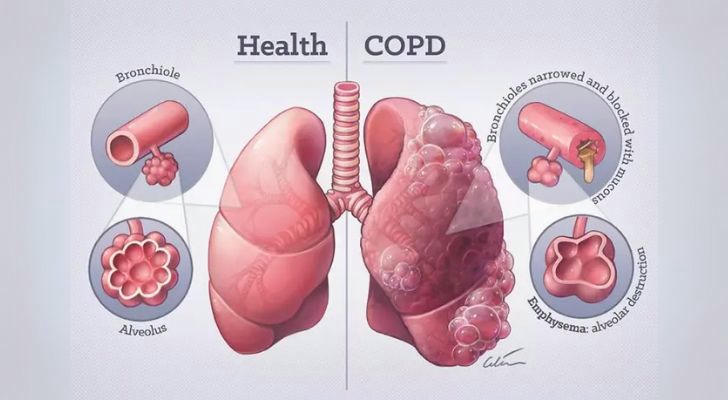
Chronic Obstructive Pulmonary Disease (COPD) is a progressive lung condition that restricts airflow and makes breathing difficult. It includes chronic bronchitis and emphysema, both of which damage the lungs and airways. Symptoms include persistent coughing, wheezing, shortness of breath, and frequent respiratory infections. According to the CDC, over 16 million Americans have been diagnosed with COPD, and millions more likely remain undiagnosed.
COPD is most commonly caused by long-term exposure to irritants such as cigarette smoke, air pollution, chemical fumes, or dust. While it cannot be cured, early diagnosis and innovative treatments can significantly improve quality of life.
Stages of COPD and Their Characteristics
Understanding the stages of COPD helps guide treatment strategies and predict progression. COPD is typically classified using the GOLD (Global Initiative for Chronic Obstructive Lung Disease) staging system, based on symptoms and lung function (FEV1 scores).
| Stage | FEV1 (% Predicted) | Key Symptoms | Functional Impact |
|---|---|---|---|
| Mild (Stage I) | ≥ 80% | Occasional shortness of breath, mild cough | Little or no limitation in activity |
| Moderate (Stage II) | 50–79% | Frequent cough, shortness of breath during activity | Reduced exercise tolerance |
| Severe (Stage III) | 30–49% | Breathlessness with minimal activity, fatigue | Significant limitation in daily tasks |
| Very Severe (Stage IV) | < 30% or < 50% with chronic respiratory failure | Life-threatening exacerbations, severe breathlessness | Poor quality of life, frequent hospitalizations |
Popular COPD Treatment Methods and Medical Procedures
Traditional treatments include lifestyle changes and medications, but today's approaches are evolving rapidly. Here's a comprehensive look at both established and innovative therapies in 2025:
1. Bronchodilators and Inhaled Corticosteroids
- Purpose: Relax airway muscles and reduce inflammation.
- Examples: Albuterol, Tiotropium, Salmeterol, Fluticasone.
- Usage: Daily maintenance or emergency relief.
2. Pulmonary Rehabilitation
- Components: Supervised exercise training, nutrition advice, and education.
- Outcome: Improves stamina and reduces symptom severity.
3. Oxygen Therapy
- For: Patients with low blood oxygen levels.
- Technology: Portable oxygen concentrators allow for mobility.
4. Lung Volume Reduction Surgery (LVRS)
- Description: Removes damaged lung tissue to improve breathing mechanics.
- Candidates: Patients with upper-lobe emphysema and low exercise capacity.
5. Lung Transplant
- Reserved for: End-stage COPD patients with very poor lung function.
- Challenges: Limited donors, high costs, lifelong immunosuppression.
6. Minimally Invasive Procedures
- Endobronchial Valves: One-way valves inserted into airways to redirect airflow, improving lung function.
- Targeted Lung Denervation (TLD): Experimental technique reducing nerve signals to prevent airway constriction.
7. Regenerative Medicine & Stem Cell Therapy
- Current status: Clinical trials underway.
- Goal: Regenerate damaged lung tissue using stem cells or biologics.
- Potential: Could slow progression or partially reverse damage.
8. Digital Health & AI Tools
- Tools: Smart inhalers, remote monitoring, AI-assisted diagnostics.
- Benefits: Real-time data on medication adherence and early warning of exacerbations.
Real Case: Breaking Barriers with Endobronchial Valves and Digital Monitoring

Patient: Mary Thompson, 67, former smoker, diagnosed with GOLD Stage III COPD in 2021.
Pre-treatment FEV1: 38% predicted
Symptoms: Could walk only 200 feet before breathlessness, frequent hospitalizations (4 times/year).
Treatment Plan (2023–2025):
- Implanted endobronchial valves in her left upper lung (minimally invasive procedure)
- Started using a smart inhaler synced with a mobile app to track daily usage
- Enrolled in a remote digital health program with her pulmonologist
Outcomes After 12 Months:
- FEV1 improved to 48% predicted
- 6-minute walk distance increased to 1,000 feet
- Hospital visits dropped to 1/year
- Quality of life score (SGRQ) improved from 65 to 42
Mary describes the change as “life returned to normal.” Her pulmonologist notes this hybrid of procedure and tech is a model for managing COPD in the future.
Table: Treatment Innovations and Effectiveness Comparison
| Treatment Method | Innovation Level | Average Improvement in FEV1 | Impact on Hospitalizations | Availability |
|---|---|---|---|---|
| Inhalers (Combo) | Traditional | +5–10% | Moderate reduction | Widely available |
| Pulmonary Rehab | Standard | No direct FEV1 change | Significant QoL improvement | Available nationwide |
| Endobronchial Valves | Innovative | +10–15% | Major reduction | Select hospitals |
| Lung Transplant | Last resort | +50–70% | Elimination (if successful) | Limited access |
| Digital Monitoring | Innovative | Indirect benefit | Early exacerbation detection | Expanding coverage |
| Stem Cell Therapy | Experimental | Unknown | Unknown | Clinical trials only |
FAQs
1. Can COPD be cured?
No, COPD is irreversible, but modern treatments can slow its progression and improve quality of life.
2. What are the most promising new treatments for COPD?
Endobronchial valves, targeted lung denervation, and AI-powered inhalers are leading the innovation wave.
3. How do I know what stage of COPD I have?
A pulmonary function test (PFT), especially measuring FEV1, helps determine your stage. Always consult with a pulmonologist.
4. Are these new treatments covered by insurance?
Many treatments, like bronchodilators and pulmonary rehab, are covered. Procedures like valve implants may require special authorization. It's best to check with your provider or explore financial assistance via programs like Medicare.
5. Is exercise safe with COPD?
Yes — under supervision. Pulmonary rehab programs are specifically designed to help COPD patients build strength safely.
Conclusion
The landscape of COPD treatment is transforming faster than ever. While traditional methods still play a vital role, today’s innovations — from smart devices to minimally invasive surgeries — are reshaping how this chronic disease is managed. For patients like Mary, the integration of new technologies and medical procedures offers more than just symptom relief — it offers hope.
Early diagnosis, personalized treatment, and access to innovative care can change the story of COPD from one of decline to one of possibility. Talk to your healthcare provider about which advanced options may be right for you.
Keywords:
COPD | lung function | bronchodilators | endobronchial valves | pulmonary rehabilitation | oxygen therapy | FEV1 | regenerative medicine | smart inhalers | chronic obstructive pulmonary disease
